Your gut’s bustling microbial metropolis may hold the keys not just to digestion, but to your happiness, anxiety, and even your risk of mental illness—if the latest science is to be believed.
Story Highlights
- Cutting-edge research reveals a two-way street between gut bacteria and brain function, with trillions of microbes potentially influencing mood, anxiety, and serious mental disorders.
- Recent meta-analyses show probiotics and dietary changes can modestly but significantly reduce symptoms of depression and anxiety—though effects vary and are not yet a cure-all.
- Harvard and Stanford teams are leading efforts to decode the biological pathways—inflammation, immune signals, and nerve connections—linking gut health to mental health.
- The field is moving fast, with large clinical trials underway, but experts caution that most human evidence is still correlational, and personalized approaches will be key.
- For now, probiotics and gut-friendly diets are adjunct tools, not replacements, for traditional mental health treatments—but the promise of a microbiome revolution in psychiatry is real.
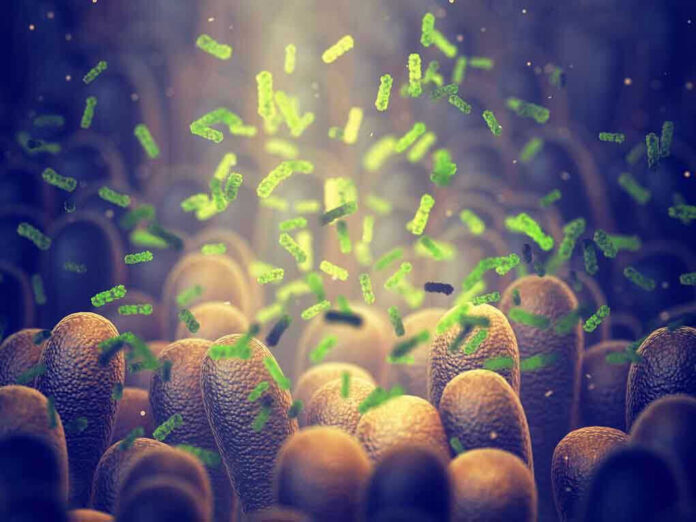
The Gut-Brain Axis: More Than a Gut Feeling
The idea that your intestines talk to your brain isn’t new—ancient healers suspected it, and 19th-century neurologists documented “nervous stomachs.” But only in the last 20 years, with DNA sequencing and advanced imaging, has science mapped the gut-brain axis in detail: a complex network of neurons, hormones, and immune signals shuttling messages between your belly and your skull[3]. Animal studies in the early 2000s showed that tweaking gut bacteria could alter behavior and stress responses. By the 2010s, human studies began linking specific microbial profiles to anxiety, depression, even schizophrenia and bipolar disorder[2].
From Correlation to Causation: What the Data Really Say
Meta-analyses published in 2025 confirm that people with depression or anxiety often have different gut microbiomes than healthy controls, and that probiotics—live bacteria taken as supplements or in food—can reduce symptoms, especially in depression and anxiety[1][2]. The effects are real, but modest: no one is claiming a miracle cure. Clinical trials are now testing which strains, doses, and diets work best, for whom, and why. Some studies suggest that inflammation triggered by certain gut bacteria—like Morganella morganii, flagged in a Harvard study—may directly contribute to depressive symptoms[4]. Others point to the vagus nerve, a biological superhighway connecting gut and brain, as a critical messenger[3].
Hope, Hype, and Hard Realities
The explosion of interest has led to a probiotics gold rush, with companies and clinics touting microbiome fixes for mental health. But top researchers—including teams at Harvard and Stanford—urge caution. While animal studies show clear cause-and-effect, most human evidence remains correlational. Not everyone responds to probiotics, and effects are often small. The field lacks precise biomarkers to predict who will benefit, and long-term safety data are scarce[2]. For now, microbiome modulation is an adjunct, not a replacement, for proven therapies like medication and talk therapy. Yet for patients with treatment-resistant conditions, even modest new options are welcome.
Who Stands to Gain—and Who Calls the Shots
Patients with stubborn depression, anxiety, or psychosis are the most obvious beneficiaries, but the implications ripple out. Clinicians gain new tools, especially for cases where standard treatments fail. Pharmaceutical and biotech firms see a lucrative new market in probiotics, prebiotics, and microbiome diagnostics. Academic researchers chase grants and glory in a hot, interdisciplinary field. Regulators like the FDA must weigh hope against evidence, ensuring new therapies are safe and effective before they reach the public. Patient advocacy groups, meanwhile, push for faster progress and broader access.
The Future of Mental Health: Personalized Bugs?
If the science holds, the next decade could see a shift toward personalized mental health care based on your unique microbial fingerprint. Researchers envision stool tests guiding probiotic prescriptions, dietary plans tailored to your gut flora, and even fecal transplants—already used for gut infections—being tested for psychiatric disorders. But major hurdles remain: large, rigorous trials are needed to prove which interventions work, for whom, and why. The gut-brain axis is a promising frontier, but it’s no panacea—yet[2].
Expert Voices: Optimism Tempered by Pragmatism
Leading scientists agree the gut-brain connection is real and important, but stress that hype must not outpace evidence. Meta-analyses and systematic reviews consistently report modest benefits from microbiome interventions, especially for mood disorders, but note that study designs and results vary widely[1][2]. Some clinicians report dramatic improvements in individual patients, but emphasize that what works for one may not work for another. The consensus: stay curious, but skeptical. The gut may be a new ally in mental health, but it’s not the only one—and for now, traditional treatments remain the backbone of care.
Sources:
Meta-analysis on gut microbiome and mental health (Niger Med J, 2025)
Systematic review on gut microbiome and psychiatric disorders (PubMed, 2025)
Nature review on probiotics and mood (Nature, 2025)
Harvard Medical School study on gut bacteria and depression (Harvard, 2025)
Nature news feature on microbiota and mental health (Nature, 2025)
Stanford Medicine overview on gut-brain connection (Stanford, 2025)















